
Is Crohn's disease genetic?
January 19, 2011

- Related Topics:
- Environmental influence,
- Autoimmune disease,
- Complex traits
A curious adult from California asks:
"Is Crohn’s disease genetic?"
Thanks for asking this question! Yes, Crohn's disease is genetic but that isn't the whole story. Like with many other diseases, the environment plays a role too.
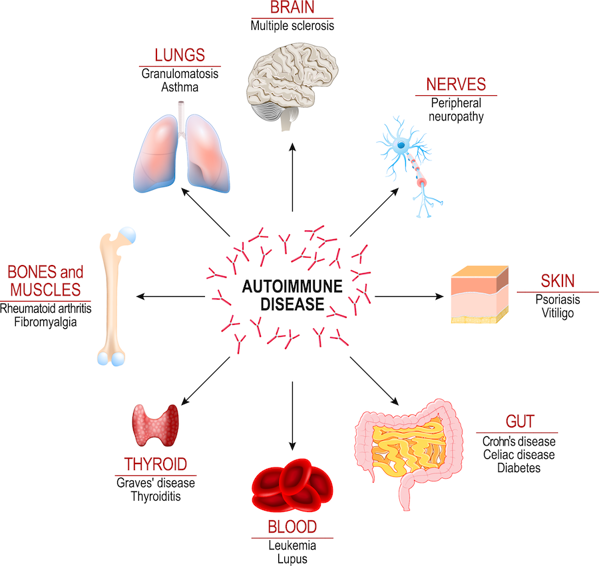
Crohn's disease affects the digestive system (usually the lower half of the small intestine and colon). People typically start to get symptoms between the ages of 15 and 30. It is thought to happen when someone's own immune system attacks his or her digestive system. This is called an autoimmune disease.
The exact cause for why a person develops Crohn's disease is unknown. However, scientists have found that it tends to cluster in families. This usually means that genes play at least some role in a disease.
Those who have a parent or sibling with Crohn's disease have a 5-10% chance of developing the disease. If both parents have Crohn’s, a child has about a 33% chance of developing the disease too.1
Despite this, Crohn's disease doesn't look to be entirely genetic. How can scientists tell? By looking at identical twins!
The Nature vs Nurture of Crohn's Disease
To figure out how big a role genes play in Crohn's disease, scientists compared identical twins. They found that if one identical twin developed Crohn's disease, the other twin has about a 1 in 3 chance of getting it too.1
If the disease was completely genetic, both twins should have the disorder 100% of time. This is because identical twins share 100% of their genes.

So Crohn's disease isn't only due to genes, but also to other outside factors that we may be able to control. These factors won't give you Crohn's disease on their own, but they can increase your risk.
While we don't know the exact cause of Crohn's disease, we do know some factors that can bring on symptoms of the disease. For example, cigarette smoke, stress, and living/working environment can increase someone's risk. So too can eating foods that are high in fat, fiber, alcohol and milk protein.2
Another possible risk has to do with the bacteria that hang out in your gut.3 Some people end up with "bad" bacteria there. Some scientists think that a person's immune system attacks these bacteria, causing Crohn's disease.
Bad diet, a broken immune system, stress, etc. all seem to contribute to Crohn's disease. But they obviously aren't enough. Not every couch potato powering through Twinkies ends up with Crohn's disease.
So, there is more to it than simply the environment. As the twin study showed, genes play an important role too.
Crohn's Disease and the Gene Card
To understand how Crohn's disease can be genetic, we need to take a step back and talk about chromosomes and genes. Our 23 pairs of chromosomes are like mini storage units for our genes. And each of these genes has the instructions for one small part of us.
As humans, we all share pretty much the same genes. What makes each of us different is that we can have different versions of the same genes. And some of these versions can make us more or less likely to end up with a disease.
To date, scientists have found changes in over 30 genes on these two chromosomes that increase the risk for a person to develop the disease.4 They've also found areas on these chromosomes that, even though they have no genes, still appear to affect someone's chances of getting Crohn's disease.
CARD15 (also known as NOD2) was one of the first genes identified in Crohn's disease.5 About 1 in 3 patients with Crohn’s disease have certain versions of this gene.4
Changes in the ATG16L1, IL23R, IRGM, and CCR6 genes also put a person at risk for developing Crohn's disease. Interestingly, all of these genes are involved in the immune system.
This makes sense since Crohn's disease is almost certainly an autoimmune disorder. People with these gene versions have immune systems that might mistake bacteria in the gut as something that needs to be attacked. Or that might even attack that person's gut itself!
Scientists have also found parts of these chromosomes that affect a person's risk for getting the disease where they don't quite know what is going on. For example, one region, called IBD5 on chromosome 5, is one of these.
There are also regions on chromosome 5 and 10 that have no known genes at all. However, these regions may determine how nearby genes work. As you can see, scientists have done a good job of collecting different parts of our DNA that affect our risk for getting Crohn's disease. Now they just need to figure out how they are involved.
While trying to understand the genetics of Crohn's disease, scientists also found that the disorder is linked to some other diseases and conditions. Studies are now looking into how they are connected.
Blood Sugar, Skin, Joints and Crohn's Disease: What's the connection?
Research now shows that there is a genetic link between Crohn's disease and diabetes, rheumatoid arthritis, and psoriasis. These other disorders are linked to blood sugar and joint and skin inflammation.
More recently, Ankylosing Spondylitis (AS), a type of arthritis that affects the spine and pelvic joints, was found to have a high incidence in Crohn's disease. Both types of disorders are linked to some of the same genes.
Interestingly, many of those shared genes are linked to the immune system. This shows how important the immune system is to these disorders and to overall body function.
As researchers learn more about the genes involved in Crohn's disease and the link to many other disorders, they may be able to come up with new ways to treat the disease(s). For example, if a person has rheumatoid arthritis and Crohn's disease, finding an anti-inflammatory drug may help the person deal with both at once.
So, hopefully you can see that Crohn's disease has a very strong genetic link. However, environment can also play a role as well. Knowing your risks and leading a healthy lifestyle can control the symptoms and decrease the likelihood of having the disorder.
Read More:
- KidsHealth: Chronic Inflammatory Bowel Disease
- HowStuffWorks: Basics of the Immune System
- Medline: Genetics of Crohn disease

Author: Dr. Khameeka Kitt
When this answer was published in 2011, Khameeka was a post-doctoral fellow in the Department of Biology, studying initiation and stabilization of epithelial cellular adhesions in James Nelson's laboratory. Khameeka wrote this answer while participating in the Stanford at The Tech program.
 Skip Navigation
Skip Navigation
