
What is currently being done about Cystic Fibrosis?
December 4, 2008

- Related Topics:
- Cystic fibrosis,
- Autosomal recessive inheritance,
- Genetic conditions
A curious adult from California asks:
“What is currently being done about Cystic Fibrosis? I have two daughters who suffer from the disease.”
I am so sorry to hear that your daughters have Cystic Fibrosis. CF is not uncommon among people of European descent. In fact, it is estimated that 1 out of every 25 of these folks are carriers for CF.1 So your daughters are not alone. But this is obviously of little comfort to you.
What you want to know are some of the upcoming treatments that will become available. And ultimately if we'll ever be able to cure CF.
Treatments for CF have certainly improved over the last 20 years. CF used to almost always be fatal in childhood. Nowadays life expectancy is upwards of 36 years.2
Scientists are working hard to find a cure. We know that CF happens because of certain changes in the CFTR gene. Over 1600 of these changes have been identified so far! Many of these changes make the gene not do its job properly.
So one idea behind a cure is to add back a copy of the CFTR gene that works well. This would make up for the poorly working gene.
Another idea is to come up with a medicine that causes the patient's CFTR gene to start working properly again. Or that at least mimics what the CFTR gene does in the lungs. Now it would be like the patient had a CFTR gene that worked well.
Scientists are investigating both approaches. Before going into depth about these treatments and cures, I want to step back a bit and go over CF in more detail. I'll talk about the CFTR gene and the symptoms of the disease. Once we understand those, then we can explore upcoming treatments and potential cures.
Changes in the CFTR Gene Cause CF
Back in 1989, the gene responsible for CF was identified. Its name is CFTR.3
Remember, genes are simply the instructions for a protein. And a protein is a sort of molecular machine that does a job in the cell.
The CFTR gene makes a protein that sits on the outside of cells. This protein helps chloride molecules get from the outside to the inside of cells.
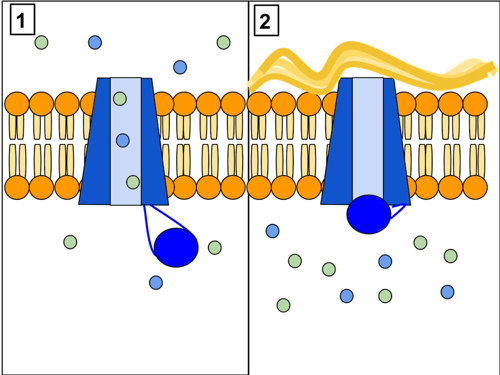

The different changes in the CFTR gene that can cause CF change its instructions so that a poorly working CFTR protein gets made. Or the protein gets stuck in the wrong place in the cell. Or no CFTR protein gets made at all.3
We still don't know why changes in this gene cause the symptoms we see in CF. But, scientists are finding ways to better treat these symptoms. Click here to find out about some of these.
Again, remember that the treatments found at that link only treat the symptoms of the disease. Since this disease is genetic, what we really want to do is cure it with a working gene. Or at least find a medicine that gets these cells to make working CFTR protein again.
Making a Gene Work Properly
Scientists are trying lots of different ways to get a patient's CFTR gene to work right. Because different gene changes have different effects on the protein, these "cures" will each only work for some CF cases.
One of these potential treatments/cures is a medicine known as PTC124. This medicine will only work in about 10% of patients in the U.S. But it might be able to kick-start these patients' CFTR gene into working again. And so "cure" their CF.4
Remember, a gene encodes the instructions for making a certain protein. Like a sentence, these instructions have a start and a finish. In a sentence, the start is a capital letter and the end is a period.
In a gene, starts and finishes aren't punctuation. Instead, they are certain three letter words.
The instructions of genes are written in three letter words using four different letters -- A, G, T, and C. So a gene's instructions have words like AGA, TGC, TTT, etc.
Most of these words tell a cell which amino acid to add next when making a protein. (Amino acids are the building blocks of proteins). This means that a gene is really just a long list of which amino acids go where in a protein.
Some of these words (or codons as scientists call them) tell the cell when to start making a protein. The start codon is usually ATG. Other words tell a cell when to stop. The stop codons are usually TAA, TAG, or TGA.
PTC124 works by having the cell skip over a stop and so make the whole protein. Imagine the following sentence:
The CFTR protein works well.
If an extra period were put in, you'd end up with:
The CFTR.
This sentence doesn't mean anything anymore. But if we erase the period in the middle, then it makes sense again. And this is what PTC124 is supposed to do.
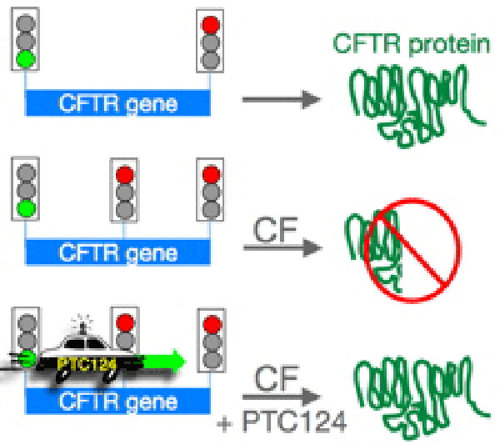

Around 10% of people of European descent have this type of change (called a nonsense mutation). For example, there is usually the word TGT at amino acid 225 in CFTR. TGT codes for an amino acid named cysteine. A single change (T to A) makes the word TGA, which is a stop codon.
People with this change often end up with CF because they don't make the whole CFTR protein. Sort of like the period in the middle of our sentence.
PTC124 has the cell skip over the stop codon. Now a much better working protein can get made. And the symptoms of CF can become much less severe.
That's the idea anyway. There are a number of clinical trials underway to test how well this drug works in CF patients. The results are promising so far. But bear in mind that many drugs still fail at this stage of testing.4
And remember that this treatment will not work for all CF patients. In fact, it won't work for the most common way to get CF, the delta F508 change.5
Proteins that come from a CFTR gene with the delta F508 change tend to get chewed up by the cell. And the little bit that remains ends up stuck in the wrong part of the cell. Scientists are working on ways to get more of the CFTR protein to the right place in people with the delta F508 change.
So each different type of gene change needs a different medicine. It would be much easier to find a treatment that works on all cases of CF. The treatment with the best shot at this is gene therapy.
Gene Therapy and CF
The idea behind gene therapy is very simple. Since some diseases are caused by changes in a single gene, giving a person just one working copy of the gene should cure it.
Sadly, while the idea is simple, there are many problems with gene therapy. Click here to learn some of the general problems scientists have run into.
Because of the type of genetic disease CF is, it was one of the first major targets for gene therapy. Unfortunately, an effective gene therapy method to cure CF still does not exist.
On top of the problems with gene therapy in general, CF itself actually complicates things. Scientists still don't fully understand why non-working copies of CFTR cause all of the disease symptoms. And it is still unclear what types of cells or tissues really need to have a working CFTR protein to cure the disease.6
Also, the damage caused by infection and inflammation, as well as the thick mucus in the lungs makes getting a working copy of the gene into the correct cells even harder. On top of all this, many of the lung cells are replaced with new ones at a very high rate. So even if a lung cell gets a working CFTR gene, the body might replace it with one that doesn't have a working CFTR.6
Don't give up hope, though! Scientists haven't. New technologies for gene therapy are being worked out. Also, in the future scientists may be able to use stem cell or other cell-based treatments to try to cure CF.
And remember, even without curing the disease at the genetic level, scientists are still working hard to make the symptoms less harmful.
Editor’s Note (5/23/2022): Treatments for CF have improved significantly in the past 14 years. New drugs include ivacaftor, lumacaftor, and ataluren, which can help approximately 50% of patients. The rest of patients have “orphan mutations” — unique mutations that are difficult to develop treatments for since they each affect a small number of people.7,8

Author: Jared Wenger
When this answer was published in 2008, Jared was a Ph.D. candidate in the Department of Genetics, studying yeast carbon metabolism and genome evolution in Gavin Sherlock's laboratory. Jared wrote this answer while participating in the Stanford at The Tech program.
 Skip Navigation
Skip Navigation
