What is the Rh factor and why is it a problem to be Rh negative during pregnancy?
March 3, 2012
- Related Topics:
- Blood type,
- Rh factor,
- Reproduction
A curious mom-to-be in California asks:
"My doctor told me that I’ll have to get a RhoGAM shot later in my pregnancy because I have type O negative blood. What is the Rh factor and why is it a problem to be Rh negative during pregnancy? And why would something that can be such a danger to a baby become as common as it is?"
The main risk for an Rh positive baby of an Rh negative mom is something called hemolytic disease of the newborn. Even though I'm describing this for Mom, it's important to note that not all families look like this one! Your biologically female parent might be called "Dad" or something else entirely. But to keep it simple, I'll refer to the female biological parent here as "Mom".
What can happen is that mom's immune system attacks and destroys some of her unborn child's blood cells. If enough blood cells are destroyed, the baby can become very sick and even die.
It is important to note that being an Rh negative mom isn't always a problem. It's only an issue if the baby is Rh positive AND the baby's blood mixes with mom's during the pregnancy.
If the biological father is also Rh negative, things are usually fine because chances are the baby will be Rh negative, too. And sometimes it isn't even an issue if dad is Rh positive. An Rh positive dad can sometimes have an Rh negative child.
Remember, that problems only happen when the baby’s blood mixes with the mom’s blood. This doesn't always happen during pregnancy. In fact, the most common way HDN happens is during childbirth. This is one of the reasons why second and later children are at a higher risk for HDN than a firstborn child. (Keep in mind, though, that a firstborn is at risk too!)
Luckily, scientists came up with a solution to this problem back in the 1960's called RhoGAM. RhoGAM sops up Rh positive cells that may have escaped out of the baby's blood. This prevents the mom's immune system from making its own antibodies against the baby's Rh positive cells, which therefore offers protection to the unborn baby's blood cells.
To understand how all of this works, we need to take a step back and go over what Rh blood type is, how it's passed down, and how our immune system works. Then we'll be able to see why Rh negative moms can pose a risk for their Rh positive babies, and how RhoGAM keeps the baby safe.
Red Blood Cell Decorations
Our blood types are described mostly by two things – ABO group and the Rh factor. Both of these describe labels that "decorate" the outside of our red blood cells. Here, we'll talk mostly about the Rh factor, but you can learn more about the ABO system here.
The Rh factor was first discovered in the 1940's when red blood cells from a Rhesus macaque monkey were injected into a rabbit. The scientists who did this found that the rabbit's blood cells clumped together. This happened because the rabbit's blood had antibodies that reacted with something in the monkey's blood. That something was named the "Rhesus" or "Rh" factor.
Rh positive people have a "decoration" on their red blood cells called the D antigen. Rh negative people do not. "And having the D antigen may cause problems for an Rh negative pregnant person who is carrying an Rh positive baby."
Attack the Foreigner
Our bodies have a powerful defense system to protect us from the outside world, called the immune system. Immune cells work to detect anything that doesn't look like ourselves and try to get rid of it before it can harm us.
One way it does this is to make antibodies against anything that looks foreign. Antibodies act like flags that our immune cells use to find things that need to be destroyed.
People who are Rh negative don't make the D antigen. So if the D antigen is introduced into their blood, their immune system will perceive the D antigen as foreign (which it is, to them) and make antibodies against it.
These antibodies search for anything that is displaying D antigen and target it for destruction. Unfortunately this includes the Rh positive red blood cells of an unborn child.
This is called "Rh incompatibility." It can happen when an Rh negative person receives a transfusion of Rh positive blood, but this is pretty rare. The more common problem is the one that can happen during pregnancy.
Rh Negative Mom, Rh Positive Child
To understand how an Rh negative person can have an Rh positive child, we need to understand how those decorations (antigens) we talked about end up on the outside of our blood cells. They are there because of the specific genes we carry.
You probably already know that we have two sets of genes in most of our cells, one set from mom and one from dad. One of these 20,000 or so genes in our cells has the information needed to make the D antigen.
There are two versions, or alleles, of this gene: one that actually makes the D antigen and one that can't. You can probably guess that Rh positive people have the first kind of allele and Rh negative people have the other one.
What you might not have guessed is that people with a copy of each allele are Rh positive, too. This makes sense since they make some D antigen because of their one copy that can make it. This is why the Rh positive allele is "dominant" over the Rh negative one. Let's see why this matters.
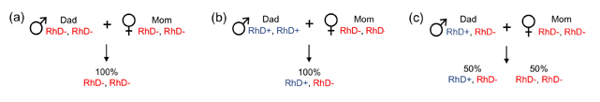
Imagine an Rh negative mom is having a baby with an Rh negative dad. Both have two copies of the Rh negative allele, and so they can only pass those on to their child. All their kids will almost certainly be Rh negative. But it isn't so clear cut if dad is Rh positive.
If dad has two copies of the Rh positive version, then all of their kids will be Rh positive. Dad will pass down an Rh positive allele and mom will pass down an Rh negative one. All the kids will have one of each and so will be Rh positive.
If dad has one copy of each allele instead, then each child has a 50% chance of being Rh negative. This is because half the time dad will pass down the Rh positive gene version, and half the time he will pass down the negative one.
But whether an Rh positive dad has one or two copies of the Rh positive allele, it's still important for an Rh negative mom to get a RhoGAM shot. This is because of something called sensitization.
Primed and Ready
Rh incompatibility problems start if any of the baby's red blood cells leak into mom's blood during pregnancy or childbirth. As I said earlier, if this happens, the mom's immune system starts making antibodies against the D antigen. Those antibodies start flagging the baby's cells for destruction.
This response is much worse for Rh negative moms who are pregnant with their second Rh positive baby. This is because it's rare for mom's body to make enough antibodies to hurt the baby during a first pregnancy. But if a second Rh positive pregnancy happens, those antibodies are already hanging around in mom's blood and ready to attack. Mom has been "sensitized" to the D antigen by her first Rh positive pregnancy.
The way we avoid sensitization is with RhoGAM. The antibodies in RhoGAM destroy any of the baby's Rh positive cells in mom's blood before her immune system has a chance to make its own antibodies. And since the antibodies in RhoGAM are a special kind that can't cross the placenta (unlike the ones that our bodies make), the baby can't be harmed by them.
Being Rh Negative Is Normal
Having a set of genes that could harm your children seems very strange. It's so strange that people are desperate to come up with wild theories about where the Rh factor came from.
Some claim that we humans got the Rh factor gene from the gods or some species of reptiles. Others claim that it came from Neanderthals. While the last option is more likely than the other two, the part of a Neanderthal's DNA where the Rh factor gene would be hasn't been looked at yet. So right now there is absolutely no evidence that we got the Rh factor from them.
The Rh negative allele is really no different than the allele that leads to blue eyes or red hair. All three are genes that have been damaged to such an extent that they no longer work.
What is really weird is that something with such obviously negative consequences spread throughout the population so that 15% of people are now Rh negative. This pretty much only happens if something negative has a positive side to it, too. An example is sickle cell anemia and malaria resistance.
Scientists aren't sure yet what the upside is of being Rh negative, but a recent idea is that it may protect from a parasite called Toxoplasma gondii. It doesn't keep you from getting the parasite, but it might make the effect less severe.
Toxoplasma gondii affects people's motor skills. For example, it seems to slow down people's responses so they are more likely to get in car accidents.
A couple of recent studies showed that having one copy of each Rh allele protects someone from these effects. In other words, people with one Rh positive copy and one Rh negative copy may do better in areas with lots of Toxoplasma gondii infections. Like in Europe, for example, where being Rh negative is much more common than other places in the world.
Whatever the benefit, we can see by looking at human DNA that having the Rh negative allele is perfectly normal. A chunk of DNA went missing sometime during evolution, the way these things sometimes do.
And now that we have RhoGAM, we don't have to worry about all of the disadvantages of being Rh negative anymore. Since it's been widely used during pregnancy, the Rh positive babies of Rh negative moms aren't usually at risk.

Author: Dr. Maggie Pearce
When this answer was published in 2012, Maggie was a postdoctoral fellow in the Department of Biology, studying protein quality control and neurodegeneration in Ron Kopito's laboratory. Maggie wrote this answer while participating in the Stanford at The Tech program.
 Skip Navigation
Skip Navigation
