How is hypertrophic cardiomyopathy passed on?
June 22, 2016
- Related Topics:
- Medical genetics,
- Complex traits
An undergraduate student from Australia asks:
“I have a genetic heart condition called apical hypertrophic cardiomyopathy. Both my parents and my brother are not affected by this condition however it seems one of my father’s mother’s brothers was.
Is it genetic? If so, how is it passed on?”
Hypertrophic cardiomyopathy or HCM is a common heart condition (about 1 in 500 people has it) that is often genetic. But how it is passed down is not so simple.
Most cases happen because something has gone a bit wrong with a heart muscle gene (more about that later). If either your mom or your dad passes that gene to you, you could end up with HCM. Geneticists call this sort of thing “autosomal dominant.”
Sounds simple but here is where it gets a bit tricky. Sometimes you can get that copy of the gene that isn’t working right and still not get HCM. That’s called “incomplete penetrance.”
So sometimes a parent might have the gene that causes HCM but not have HCM. But then their child gets the gene and ends up with HCM. This might explain why you have it but your parents don’t.
Another possibility is that a genetic change happened only in you, which was not inherited from your parents. This sort of thing happens often enough that it has its own name — de novo. So this might be another reason you have it and your parents don’t.

HCM can also develop over time not because of a genetic change, but because of other health factors like high blood pressure or aging.
I know, it is complicated. But you asked! Let’s break it down in a little more detail …
The Muscles in the Heart
First, let’s understand what we mean by genes: genes are the set of instructions that make you, you! Genes are pieces of DNA that are specific instructions for your body. Some genes, many in fact, are the instructions your body needs to correctly build muscle.
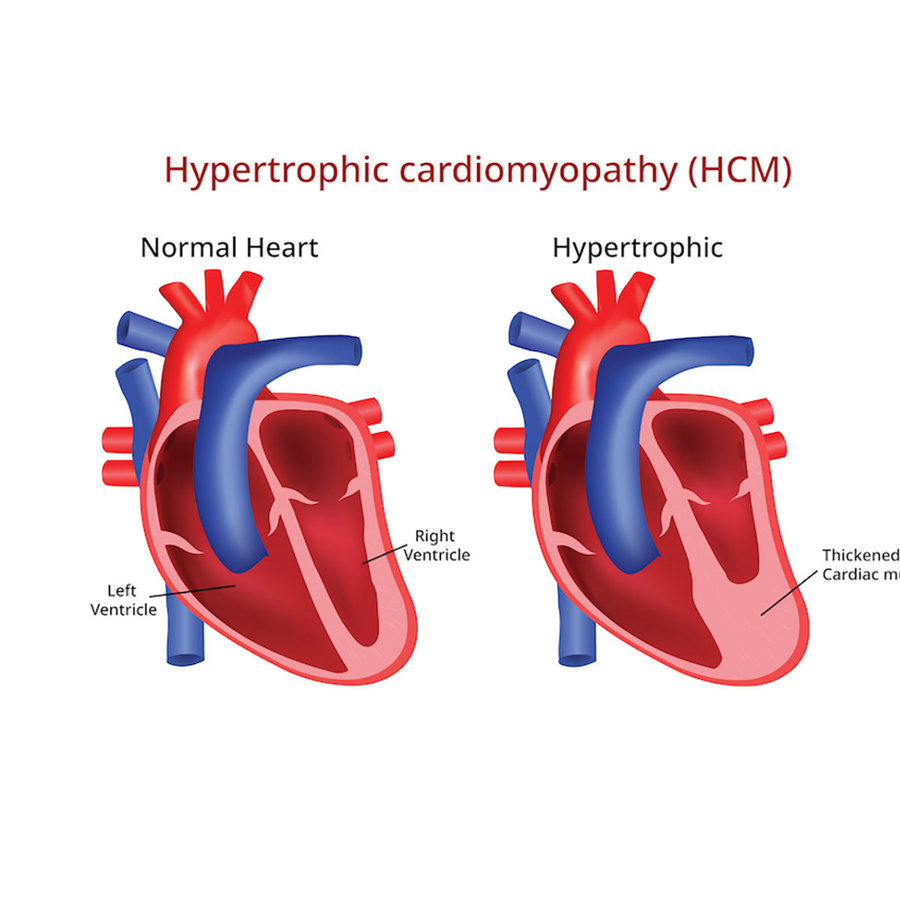
And as you can see in the image below, you don’t have just one type of muscle:
There is muscle that helps you move (skeletal muscle) as well as muscle that moves food through digestion (smooth muscle) and makes your heart pump (cardiac muscle).
All muscle, including heart muscle, is made of many parts put together in a very organized way. Some parts of the muscle move, some parts anchor to one place, all to allow it to expand and contract in an orderly way. All of these pieces of muscle are created from the instructions of special muscle genes.
If there are any mistakes in the gene for one of these muscle pieces, then there may be problems with the muscle that develop over time.
The Nuts and Bolts of HCM
One such problem is the condition you asked about, hypertrophic cardiomyopathy (HCM). Let’s break down those words so we can understand what that means:
- Hyper in Greek means “more” or “extra”
- Trophic, also Greek, is the word for “nourishment” or “development”
- Cardio, Greek again, is the word for “heart”
- Myo, you guessed it, from Greek, means “muscle”
- Pathy in Greek indicates disease
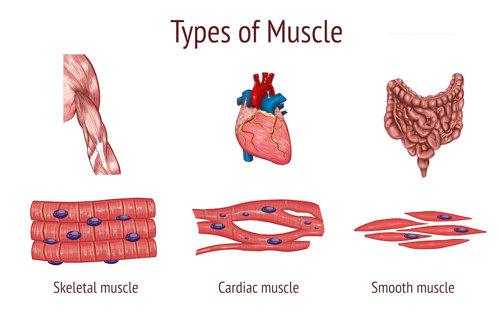
Taken together, hypertrophic cardiomyopathy means a disease of extra tissue of the heart muscle that often looks like this:
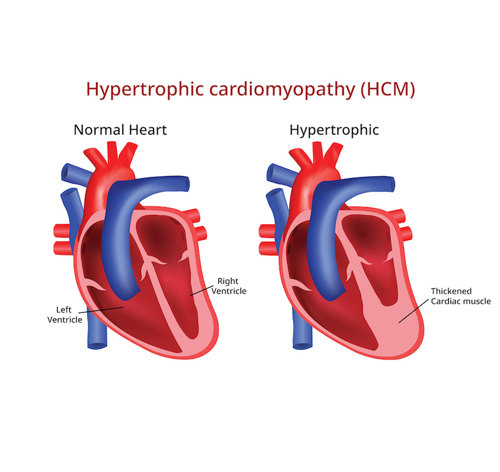
More often than not, it’s extra, thickened muscle on the left side of the heart, called the left ventricle.
The reason this thickening can cause disease is that the heart can’t fill as well with blood when the muscle is so thick. So each time the heart pumps, it doesn’t fill back up very much, and therefore can’t pump very much blood back out. So it has to work extra hard to pump enough blood for our body to function well.
Over time this stresses the heart and it doesn’t work as well, which can lead to very serious heart disease.
Fortunately, cardiologists (heart doctors) can look for this thickening in the heart and give special medications to help the heart not get thicker and work the best it can. With good evaluation and care of a cardiologist many people with HCM can lead fairly normal lives.
The last explanation I’ll give specific to the heart is about the word “apical” in your question. Apical refers to where in the heart there is this thickening. The bottom, pointy tip of the heart is called the apex.
So apical HCM means that the thickened heart muscle is more around the bottom of the heart. Still the same idea though: the job of the heart may be harder because it can't fill and pump as well when it's too thick.
Passing Down HCM
Alright, enough ancient Greek and physiology, now back to those genes!
There have been a handful of genes found to cause HCM. They are all instructions for the different pieces that form cardiac muscle and help to keep it organized and working right. If there's a change in one (or more) of these genes then the heart muscle can get disturbed so that over time it grows thicker and thicker.
The opposite can also be true, where changes in some of these cardiac muscle genes can cause the heart muscle to grow thinner and weaker over time. As you might imagine, this is also bad and causes disease.
These changes in cardiac muscle genes can be passed down through a family, or inherited. But again, how they are passed down can be a bit tricky to explain.
With HCM, you usually only have to get it from one parent. In genetics speak, this is called autosomal dominant.
But with HCM, sometimes you can have a gene that should cause the disease but doesn’t. So you might get a genetic change that causes HCM from one of your parents even though they don’t have it.
There are a few ways this might happen. For example, since HCM sometimes doesn’t appear until a person is middle aged, your parent might have been too young to show any signs. Sometimes HCM may never develop at all, even though that person has the genetic change that should cause it.
These two things are called age-dependent penetrance and incomplete penetrance, respectively.
Penetrance is a fancy word that means how closely the genetic change is related to developing a physical change. So age-dependent penetrance tells us that a person with this HCM genetic change may not develop HCM until they are older; incomplete penetrance means not everyone with a genetic change that should cause HCM will have the physical findings of the condition.
So, Undergrad from Australia, if you are the first person in your family to be diagnosed with HCM, it could have been a chance condition that only happened in you. Or it could be caused by a genetic change that is new in you, or inherited from your parents.
If it is new to you or not caused by something genetic, then it may not be passed on. And if you did get it from one of your parents, each of your kids would probably have a 50% chance of getting the gene that causes it from you too. But even if they get the gene, they may not end up having HCM!
Genetic Testing and HCM
With all of this you might think that a genetic test wouldn’t be worth it. But it can be.
It is important to find out about this condition as early as possible. If caught and diagnosed too late, or never diagnosed, it can cause major heart problems, disease, or even sudden death. So it's important to identify people who might be at risk for having HCM so they can work closely with a cardiologist to stay healthy.

One way to find these people is to take good, detailed family histories looking for patterns of family medical information that might be suspicious for a heart condition. In families that look to be at risk for HCM, we can do genetic testing on them to see if they carry any change that would put family members at risk for developing HCM, and follow them through their lives.
The flip side of this is letting people off the hook from being followed their whole lives by cardiology. For example, if a person comes to cardiology with apical HCM, like yourself, and the cause of HCM in this person is found on genetic testing, then we have a genetic answer for that family. We can then test other family members to see if anyone else inherited this genetic change.
If we know the answer for what is causing the HCM in the family, and find that a family member didn't inherit this change, then they don't have an increased chance to develop HCM. They don't need to be followed by cardiology any more than a normal person with no family history of HCM would. They're off the hook.
Genetic testing might be available to you to see if you carry any change we can find in the HCM genes we know about right now. If they do find something, they could then look for it in your parents, brother, and other family members to see where it came from and who has inherited it.
To do this genetic testing you can work with a genetic counselor. Genetic counselors are genetic testing experts who specialize in helping families understand and cope with this genetic information, it’s contribution to disease, and impact on the larger family.
You can find a genetic counselor in your area using the Find a Genetic Counselor tool, or one specific to Australia.

Author: Natalie Downs
When this answer was published in 2016, Natalie was a student in the Stanford MS Program in Human Genetics and Genetic Counseling. Natalie wrote this answer while participating in the Stanford at The Tech program.
 Skip Navigation
Skip Navigation
